Title:No getting lost in epilepsy~Vagus Nerve Stimulation Therapy is a brand new hope for epilepsy treatment.
Published day:2024/3/5Content
Epilepsy is a chronic disease due to the abnormal bursts of electricity to the brain neurons. It's clinically reflected as a series of uncontrollable epileptic seizures. Seizures can affect consciousness, movement, and sensation, and take many different forms. Most patients (around 40%) cannot identify the concrete root cause of seizures. In Taiwan, about 90,000 people suffer from epilepsy and epilepsy in nearly 40% of patients cannot be controlled by medication, causing patients trouble in the long term. Patients seem to have no choice but to endure unpredictable seizures and the side effects of various drugs. In 1997, the US FDA approved a new medical therapy with a device for epilepsy treatment – Vagus Nerve Stimulation Therapy (VNS) – opening a new window for patients with epilepsy.
How does a vagus nerve stimulator work?
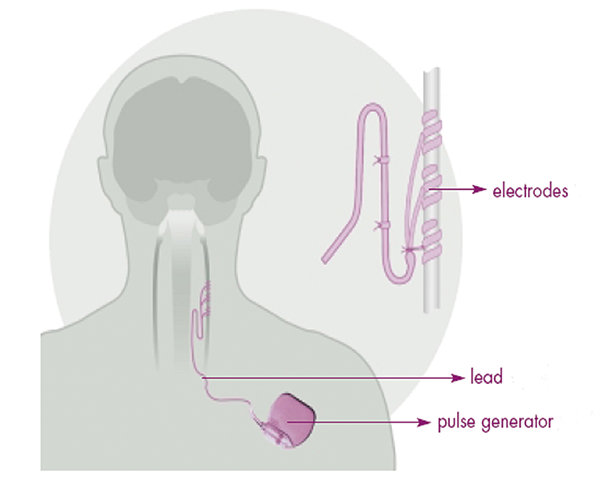
- A vagus nerve stimulator can regularly generate fixed electrical stimulation every 24 hours.
- A vagus nerve stimulator can generate and transfer electricity to the left vagus nerve through.
- A vagus nerve stimulator can help to prevent epileptic seizures induced by abnormal electrical stimulations.
Who can apply for vagus nerve stimulation?
As of the end of 2020, the whole set of "vagus nerve stimulator" medical devices were included on the list of treatments that can be reimbursed by the National Health Insurance Administration, but pre-review must be sought before use. Patients shall be assessed by the epilepsy medical team to check whether they're eligible to undergo a vagus nerve stimulator implantation. The reimbursement criteria include patients who cannot be treated by epileptic surgery or patients suffering from intractable epilepsy who have undergone surgery but failed. If the patient meets the reimbursement criteria for vagus nerve surgery, the epilepsy team will instruct the surgeon to submit an application to the National Health Insurance Administration for a vagus nerve stimulation device. If the application is approved, surgery can be arranged for the patient.
What are the steps for installing a vagus nerve stimulator in surgery?
Step 1
- The vagus nerve on the lateral side of the neck will be regularly stimulated by the electricity generated by the stimulator, which is embedded under the left clavicle or underarm.
- The second cut located on the lateral side of neck is mainly for tying the wire connector to the vagus nerve so the wire passes through under the skin and connects to the stimulator connector and the vagus nerve.
Step 2
- Adjust the factors generated by the electricity stimulations, which can be performed in the OPD. The whole step is painless. It can be adjusted with clothes on, and the patient will have regular OPD follow-ups after adjustments by a physician. The patient will only have regular OPD follow-ups later.

Conclusions:
1.Surgical effects: There have been more than 20 cases of vagus nerve stimulator implantation surgery to date. No wound infections or obvious complications after surgery have been reported. This procedure has a relatively high successful rate and the medical team can deal with potential issues effectively.
2.Surgical advantages: The surgical advantages include small-sized wounds (around 3 cm), a short surgical time (about 2 hours), and the patient can be discharged on the second day after surgery. These factors make this a convenient option for patients.
3.Follow-up treatment: The patient needs to visit the OPD for a follow-up two weeks post-surgery and have an electricity adjustment by a neurologist who specializes in epilepsy so there is a systemic follow-up treatment program in the hospital to ensure the patient receives adjustments as required.